Arthrofibrosis of the knee, ‘The Frozen knee’
What is Arthrofibrosis?
Arthrofibrosis is a complication of knee trauma or surgery, where excessive scar tissue formation and fibrous adhesions leads to a painful restriction in joint movement. It is classed as in inflammatory response and can affect all major joints. The scar tissue may form intra-articularly (inside the join) or extra-articularly (outside the joint in the soft tissue spaces). The normal healing response gets altered and leads to disordered Type 1 collagen formation. Adhesions stretch across the joint maturing into fibrous tissue. This slowly contracts and the joint capsule thickens and slowly contracts.
What are the outcomes?
Pain and restricted knee motion. This in turn leads the muscle atrophy, adaptive muscle shortening and scarring in the tissues.
How common is it?
It is more commonly seen after ACL reconstruction. In the 1980’s incidences were high at around 35%, but due to advances in surgery and a better understanding of knee rehab, incidences today are as low as 10%. Knee arthrofibrosis also affects around 1% of patients after a total knee replacement.
What are the predisposing factors?
- The injury itself: complex injuries i.e, fractures near the joint, multiple ligament injury, knee dislocations, associated meniscus tears, quads rupture, or patellar tendon rupture
- Having excessive swelling going into surgery and having very early surgery after the initial injury
- The surgery; if the ACL graft is too tight or poorly positioned. If a knee arthroplasty or a high tibial osteotomy had to be performed
- Prolonged immobilisation in a cast or brace.
- Post op complications such as infection, excessive inflammation or a haemarthrosis
- The rehabilitation; poor adherence, not getting the right advice, late mobilisation
- Genetic pre-disposal for patients who form excessive scar tissue.
Early Signs & symptoms
- Flexed knee gait
- Worsening pain
- Restricted active and passive range of movement – The patient makes early gains in ROM, but then has no further improvement. Not achieving full knee flexion/extension 2-3 weeks post operatively. The patient may lack more than 5 degrees of extension
- Weak, wasted quadriceps ; An inability to voluntarily perform a strong quadriceps contraction in the initial 1-2 weeks following knee trauma or surgery.
- Warm joint at 2+weeks
- Continued tissue swelling; the swelling associated with arthrofibrosis is in the soft tissues around the knee, giving a sensation of tissue ‘bogginess’.
- Restricted patellar mobility
- Worsening ROM – despite aggressive exercise
- No tension in the patellar tendon– patella fails to move upwards when the quadriceps contract, ie,downward migration of the patella. In an inflamed joint, there may be a transient patella infera due to fat pad and peri-patellar tissue contracture which is aggravated by quadriceps weakness. The patella may be visibly lower in position compared to the opposite normal knee. With progressing joint stiffness and limited ROM due to arthrofibrosis, the patellar tendon may permanently shorten, with the eventual onset of severe patello-femoral arthrosis.
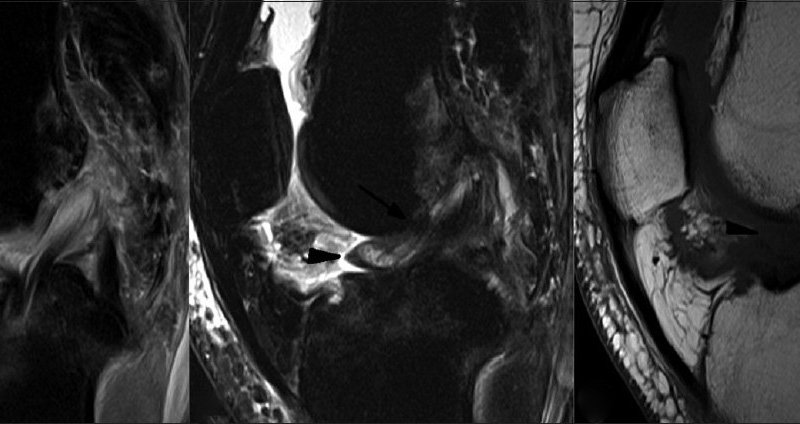
How is arthrofibrosis formally diagnosed?
The physio and the surgeon will work together to rule in knee arthrofibrosis by ruling out other mechanical or pathological knee disorders which may be blocking knee joint range. An MRI may be performed to help with a clinical diagnosis.
What can be done to avoid the onset?
- Correct surgical timing: A 1991 study by Donald Sherbourne et al in the American Journal of Sports Medicine did a study of 169 ACL reconstructions in young athletes. Those who had an early ACL reconstruction within 1 week showed a higher incidence of arthrofibrosis then those whose surgery was delayed for 3 weeks or more. This allowed time for any knee inflammation to subside pre-operatively and gave the knee a change to settle (Donald Shelbourne has also developed a knee arthrofibrosis 1-4grading system in increasing levels of severity)
- Controlling the inflammation; pre and post operatively
- Controlling the pain with analgesia to allow the patient to move pre/post operatively
- Corticosteroid injections
- NSAIDS
- Patellar (knee cap) mobilisations
- Early knee active range work pre and post-operatively.
- For ongoing arthrofibrosis; In the past manipulation under anaesthetic was used to regain knee range. These days, controlled surgical excision of the scar tissue tends to be utilised. This would normally only be done 3+ months post trauma/operation if the patient is not improving.
Final thought;
It is always worth considering arthrofibrosis as a potential diagnosis for patient struggling to regain their knee movement following the incidence of trauma or surgery. One must however remember that this is a rare condition and loss of knee extension or flexion does not always mean arthrofibrosis is the cause. Therapists and surgeons can work together to reduce the chance of knee arthrofibrosis developing and recognising it early on. This will ultimately provide the best level of patient care and help you make a full recovery
Thank you for reading,
Annika
Senior Physiotherapist
Some links for more info;
http://www.kneeguru.co.uk/KNEEnotes/courses/arthrofibrosis-12-part-course-frank-noyes-md
http://ajs.sagepub.com/content/19/4/332.short
http://link.springer.com/article/10.1007/s00402-004-0718-x
http://drmillett.com/attachments/article/87/Rehabilitation%20of%20the%20arthrofibrotic%20knee.pdf